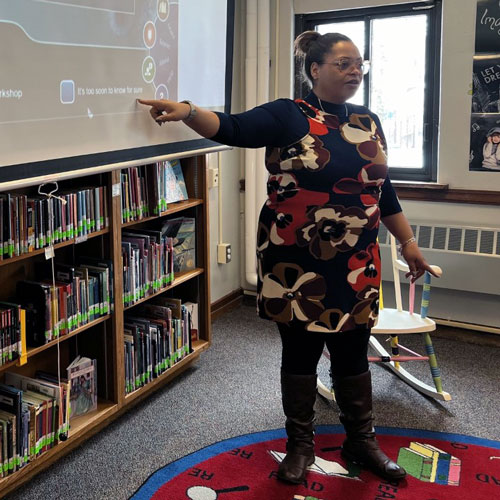
Dr. Natalie Hernandez-Green, Executive Director of the Morehouse School of Medicine Center for Maternal Health Equity, speaks with CNN about what’s being done to prevent more Black mothers from dying during or after pregnancy.

Dr. Natalie Hernandez-Green
Executive Director, MSM Center for Maternal Health Equity
By Martha Shade, CNN
ATLANTA — Kira Johnson was so excited to be a mother that she began planning her first son’s birthday party while still pregnant. The carnival-themed party she threw was epic: cake, cupcakes, and a movie poster she had printed up for the occasion.
Kira didn’t get to celebrate any birthday parties with her second son, Langston. She died hours after giving birth to him, suffering massive internal bleeding while her husband, Charles Johnson, pleaded for doctors to do something.
It’s a case so troubling it’s now taught as a cautionary tale in medical schools. And she’s just one of many.
Black women are three times more likely to die due to pregnancy than white women.
Poverty, lack of healthcare access, and obesity all play a part in the grim statistic, but that’s not the whole story; even rich, healthy, well-educated Black women face elevated risks giving birth.
Kira Johnson was a successful businesswoman, an athlete in good health, and she walked into the hospital with a supportive husband by her side.
Her life ended in the hospital, her husband says, after their pleas for help were ignored by doctors for almost 10 hours. And her husband walked out of the hospital a widow, with a newborn son in his arms.
As we celebrate Black History Month, here’s what’s being done to prevent more Black mothers from dying.
How Hospitals Can Help
Natalie Hernandez-Green, Executive Director of the Center for Maternal Health Equity at Morehouse School of Medicine, says she hears the same birthing stories over and over: Women who felt they were disrespected, whose concerns were dismissed and had birthing experiences that felt transactional and not relational.
“You want to be heard when you’re giving life. This should be the most amazing day of your life,” says Hernandez-Green.
The Center for Maternal Health Equity has partnered with local Atlanta hospitals to gather data about “Maternal Near-Misses” and see where the problems are.
Key to everything is listening to the patient, Hernandez-Green tells CNN.
“We want to respect that Black women’s voices are legitimate sources of data,” she says.
Beyond Morehouse School of Medicine’s commitment to training more Black doctors, one of the center’s approaches is to educate Patient Navigators to assist Black women, especially those who live in “maternal care deserts,” or areas without a lot of – or any — healthcare providers.
The Patient Navigators act as a bridge to doctors and other medical professionals.
They can connect women to providers – and Morehouse School of Medicine even vets those providers to make sure they provide good care to Black women.
The Patient Navigators then work alongside the pregnant woman from her first pre-natal visits to one year postpartum.
“The majority of pregnancy-related deaths happen in the postpartum period,” explains Hernandez-Green.
“More than 80% of these deaths are preventable. I always see opportunities. It’s not all gloom and doom, because there’s hope.”
Patient Navigators, Doulas, and Midwives
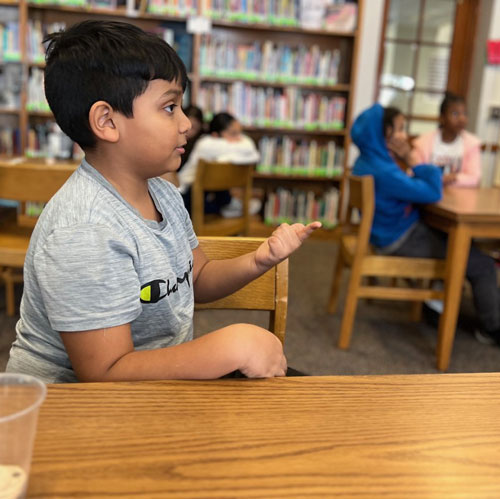
Heather Dobbs is a recent graduate of the MSM Patient Navigator program.
She had her own traumatic birth experience. Shortly after a scheduled c-section for her second child, she began to feel terrible. The anesthesiologist told her everything was fine, and she just needed fluids. Dobbs recovered briefly, then she says she began feeling “really awful” again. She said to herself: “I can’t die on this table without holding my daughter. Then I blacked out.”
When she woke up her husband, Michael, was by her side, crying. She had a port in her neck, where she had received an emergency transfusion. Doctors had performed a hysterectomy to save her life.
She was grateful to be alive but “later on, it sinks in that I was planning a larger family and now that’s not gonna happen.”
The experience made her want to help other women.
She thought about getting her nursing certification and becoming a midwife, but in the rural Georgia areas where she saw so much need, she would have had to work under an OB/GYN. And most of those areas didn’t even have doctors, so she decided to work both as a Patient Navigator and doula.
Although the roles can overlap, in general, a Patient Navigator helps patients find good care and advocates for them, while a doula actually helps a woman give birth. Many alumni of the Morehouse School of Medicine program, like Dobbs, choose to do both jobs. A midwife, in contrast, is usually a certified nurse.
As both a Patient Navigator and a doula, Dobbs follows women throughout their first year after childbirth, helping them handle the physical and mental health issues that can arise after childbirth.
April Witzel says she spent years as a labor and delivery nurse before becoming a midwife.
She has also catered to some of the most under-served parts of the state. She regularly sees women show up at the hospital right as they are about to give birth, without having had any pre-natal care, usually because they didn’t have insurance.
“I grew up poor. I’ve always thought everyone should be treated the same,” she says, explaining that her own life experience now informs much of what she does.
Witzel says she also wants to help address systemic issues that often keep Black women from accessing good care.
“When I got into healthcare, me being a Caucasian female working in a primarily African American community, I’d walk in and I’d see the look on their faces, and know they thought: ‘I don’t want her to look after me.’”
But after her patients got to know her and realized she was taking their concerns seriously, things changed.
“At the end of the day, women want to be heard, they want to trust their provider in the most vulnerable time of their lives.”
Many doctors are supportive of the additional help provided by midwives and doulas – as long as medical help is nearby when needed.
“I think there’s a place for birthing centers, midwives, doulas,” says Dr. Jocelyn Slaughter, an obstetrician and gynecologist.
“I love a good doula. I love a good midwife. Birthing centers are getting more safe; it’s good for patients that are low-risk,” says Dr. Slaughter.
CNN Anchor Abby Phillip recently opened up about why she opted for the combination of doula and a midwife when she gave birth during the pandemic. As she explained in a CNN editorial, she is a “a huge believer in modern medicine and someone who takes no unnecessary risks with my health” but she says she joined the growing group of Black women looking for more options.
Many women in the US often work all the way up until they give birth, usually in order to save up vacation days for after their child is born.
But Dr. Slaughter says that practice can be especially dangerous for Black women.
“I always say: ‘You know you’re not about to go on vacation, right?’”
“What if I told you in two weeks, you’re going to run a marathon, you’re going to give two pints of blood, and after the marathon we’re gonna wake you up every two hours?”
“Don’t you need a break before you go through this cardiac stress?” asks Dr. Slaughter.
Dr. Slaughter says she encourages her patients to take maternity leave by 37 weeks, to reduce their chances of developing conditions like pre-eclampsia, a condition that can be life-threatening.
“They’re working till the end, stressed out, feet swollen… so now they’re getting pre-eclampsia. I feel like my patients have a little lower rate of pre-eclampsia because I encourage them to start maternity leave by 37 weeks.”
While Dr. Slaughter is realistic that not everyone can afford to take that time off, she says when it’s possible, it can provide better outcomes for the mother and the baby.
Systemic Racism
Dr. Slaughter says people don’t like to talk about one of the main reasons Black women often receive inadequate care during and after pregnancy.
Slaughter says the lasting legacy of slavery and racism in the United States continues to affect Black women in all settings, including in health care.
“Because of that history, there are so many racial biases and so many socio-economic problems that women have had to fight through,” she says.
Dr. Slaughter says she believes Black women should be treated as more fragile than other women during pregnancy (and for the first year after they give birth).
“My piano teacher always told me being pregnant is like having one foot in the grave and one foot on a banana peel,” referring to all the potential perils of pregnancy.
“Black women in general have been looked at as these strong women… That’s all doctors; it’s not just white doctors. Black women are not stronger than others. They’re not.”
Dr. Slaughter says because of that misconception, doctors may miss cardiac issues happening in Black women.
The bottom line for Dr. Slaughter: “Black women need to be overly protected during pregnancy.”
How Doctors Can Help: Run That Extra Test
Dr. Slaughter also recommends medical providers remember that Black women’s bodies don’t always follow the rules in medicine “because the rules were not based upon their bodies.”
Many of the criteria for different medical diagnoses were based upon white men or white women.
“Blood pressure cut-offs, anemia levels, were not established with Black women in mind,” she says.
“I am not suggesting we get new criteria, but I do urge doctors to listen to Black pregnant women and err on the side of extreme caution when discharging or dismissing symptoms or complaints. Sometimes they know their bodies better than our medical school books.”
Kira’s Legacy
After his wife passed away, Charles Johnson pledged her death would not be in vain.
He has testified before Congress twice, helping to pass the Preventing Maternal Deaths Act in 2018 and then advocating for the Black Maternal Health Momnibus Act of 2021.
He still prints up a movie poster for each of his son’s birthdays. It’s a small nod to Kira, the family tradition she started, and the birthday parties she would have loved to have been planning for them.
Langston Johnson turned 7 last April. His dad threw him a big party with a Super Mario-themed birthday cake.
READ the article https://www.msm.edu/RSSFeedArticles/2024/February/Black-Maternal-Safety.php