prostate Cancer
Regular screenings can help early detection leading to higher success rates in treatment.
prostate Cancer
early detection saves lives
Regular screenings can help early detection leading to higher success rates in treatment.
What is prostate Cancer?
- Prostate cancer begins when cells in the prostate gland start to grow out of control. The prostate is a gland found only in males. It makes some of the fluid that is part of semen.
- The prostate is below the bladder (the hollow organ where urine is stored) and in front of the rectum (the last part of the intestines). Just behind the prostate are glands called seminal vesicles that make most of the fluid for semen. The urethra, which is the tube that carries urine and semen out of the body through the penis, goes through the center of the prostate.
- Prostate cancer is the most common cancer among men (after skin cancer), but it can often be treated successfully.
- The size of the prostate can change as a man ages. In younger men, it is about the size of a walnut, but it can be much larger in older men.
symptoms
- Eating or sleeping too much or too little
- Pulling away from people and usual activities
- Having low or no energy
- Feeling numb or like nothing matters
- Having unexplained aches and pains
- Feeling helpless or hopeless
- Smoking, drinking, or using drugs more than usual
- Feeling unusually confused, forgetful, on edge, angry, upset, worried, or scared
- Yelling or fighting with family and friends
- Experiencing severe mood swings that cause problems in relationships
- Having persistent thoughts and memories you can’t get out of your head
- Hearing voices or believing things that are not true
- Thinking of harming yourself or others
- Inability to perform daily tasks like taking care of your kids or getting to work or school
If you have any of the following symptoms, be sure to see your doctor right away.
- Difficulty starting urination.
- Weak or interrupted flow of urine.
- Urinating often, especially at night.
- Trouble emptying the bladder completely.
- Pain or burning during urination.
- Blood in the urine or semen.
Risk Factors
- Age – Prostate cancer is rare in men younger than 40, but the chance of having prostate cancer rises rapidly after age 50. About 6 in 10 cases of prostate cancer are found in men older than 65.
- Race/Ethnicity – Prostate cancer develops more often in African American men and in Caribbean men of African ancestry than in men of other races. And when it does develop in these men, they tend to be younger. Prostate cancer occurs less often in Asian American and Hispanic/Latino men than in non-Hispanic whites. The reasons for these racial and ethnic differences are not clear.
- Geography – Prostate cancer is most common in North America, northwestern Europe, Australia, and on Caribbean islands. It is less common in Asia, Africa, Central America, and South America. The reasons for this are not clear. More intensive screening for prostate cancer in some developed countries probably accounts for at least part of this difference, but other factors such as lifestyle differences (diet, etc.) are likely to be important as well. For example, Asian Americans have a lower risk of prostate cancer than white Americans, but their risk is higher than that of men of similar ethnic backgrounds living in Asia.
- Family History – prostate cancer seems to run in some families, which suggests that in some cases there may be an inherited or genetic factor. Still, most prostate cancers occur in men without a family history of it. Having a father or brother with prostate cancer more than doubles a man’s risk of developing this disease. (The risk is higher for men who have a brother with the disease than for those who have a father with it.) The risk is much higher for men with several affected relatives, particularly if their relatives were young when the cancer was found.
Ways to Prevent
- Get to and stay at a healthy weight.
- Keep physically active.
- Follow a healthy eating pattern, which includes a variety of colorful fruits and vegetables and whole grains, and avoids or limits red and processed meats, sugar-sweetened beverages, and highly processed foods.
- Vitamin, mineral, and other supplements
Screening for Prostate Cancer
A blood test called a prostate specific antigen (PSA) test measures the level of PSA in the blood. PSA is a substance made by the prostate. The levels of PSA in the blood can be higher in men who have prostate cancer. The PSA level may also be elevated in other conditions that affect the prostate.
As a rule, the higher the PSA level in the blood, the more likely a prostate problem is present. But many factors, such as age and race, can affect PSA levels. Some prostate glands make more PSA than others.
PSA levels also can be affected by:
Certain medical procedures.
Certain medications.
- An enlarged prostate.
- A prostate infection.
Digital rectal examination (DRE) is when a health care provider inserts a gloved, lubricated finger into a man’s rectum to feel the prostate for anything abnormal, such as cancer.
Prostate Cancer Stages

Following a prostate cancer diagnosis, staging is used to describe the extent of the disease. Prostate cancer staging is vital because it is used to guide the treatment plan and predict the patient’s prognosis.
The AJCC TNM staging system
A staging system is a standard way for the cancer care team to describe how far a cancer has spread. The most widely used staging system for prostate cancer is the AJCC (American Joint Committee on Cancer) TNM system, which was most recently updated in 2018.
The TNM system for prostate cancer is based on 5 key pieces of information:
- The extent of the main (primary) tumor (T category)
- Whether the cancer has spread to nearby lymph nodes (N category)
- Whether the cancer has spread (metastasized) to other parts of the body (M category)
- The PSA Level at the time of diagnosis
- The Grade Group (based on the Gleason score), which is a measure of how likely the cancer is to grow and spread quickly. This is determined by the results of the prostate biopsy (or surgery)
*There are 2 types of T categories for prostate cancer:
The clinical T category (written as cT) is your doctor’s best estimate of the extent of your disease, based on the results of the physical exam (including a digital rectal exam) and prostate biopsy, and any imaging tests you have had.
If you have surgery to remove your prostate, your doctors can also determine the pathologic T category (written as pT). The pathologic T is likely to be more accurate than the clinical T, as it is done after all of your prostate has been examined in the lab.
Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced. Once the T, N, and M categories have been determined, this information is combined (along with the Grade Group and PSA level if they are available) in a process called stage grouping to get the overall stage of the cancer.
The main stages of prostate cancer range from I (1) through IV (4). Some stages are split further (A, B, etc). As a rule, the lower the number, the less the cancer has spread. A higher number, such as stage IV, means cancer has spread more. And within a stage, an earlier letter means a lower stage. Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
diagnosis
- A biopsy is a procedure that can be used to diagnose prostate cancer. A biopsy is when a small piece of tissue is removed from the prostate and looked at under a microscope to see if there are cancer cells.
- A Gleason score is determined when the biopsy tissue is looked at under the microscope. If there is cancer, the score indicates how likely it is to spread. The score ranges from 2 to 10. The lower the score, the less likely it is that the cancer will spread.
- A biopsy is the main tool for diagnosing prostate cancer, but a doctor can use other tools to help make sure the biopsy is made in the right place. For example, doctors may use transrectal ultrasound or magnetic resonance imaging (MRI) to help guide the biopsy. With transrectal ultrasound, a probe the size of a finger is inserted into the rectum and high-energy sound waves (ultrasound) are bounced off the prostate to create a picture of the prostate called a sonogram. MRI uses magnets and radio waves to produce images on a computer. MRI does not use any radiation.
treatment
Different types of treatment are available for prostate cancer. You and your doctor will decide which treatment is right for you.
Expectant management. If your doctor thinks your prostate cancer is unlikely to grow quickly, he or she may recommend that you don’t treat the cancer right away. Instead, you can choose to wait and see if you get symptoms in one of two ways:
Active surveillance. Closely monitoring the prostate cancer by performing prostate specific antigen (PSA) tests and prostate biopsies regularly and treating the cancer only if it grows or causes symptoms.
Watchful waiting. No tests are done. Your doctor treats any symptoms when they develop. This is usually recommended for men who are expected to live for 10 more years or less.
Surgery. A prostatectomy is an operation where doctors remove the prostate. Radical prostatectomy removes the prostate as well as the surrounding tissue.
Radiation therapy. Using high-energy rays (similar to X-rays) to kill the cancer. There are two types of radiation therapy:
External radiation therapy. A machine outside the body directs radiation at the cancer cells.
Internal radiation therapy (brachytherapy). Radioactive seeds or pellets are surgically placed into or near the cancer to destroy the cancer cells.
Other therapies used in the treatment of prostate cancer
- Cryotherapy. Placing a special probe inside or near the prostate cancer to freeze and kill the cancer cells.
- Chemotherapy. Using special drugs to shrink or kill the cancer. The drugs can be pills you take, or medicines given through your veins, or, sometimes, both.
- Biological therapy. Works with your body’s immune system to help it fight cancer or to control side effects from other cancer treatments. Side effects are how your body reacts to drugs or other treatments.
- High-intensity focused ultrasound. This therapy directs high-energy sound waves (ultrasound) at the cancer to kill cancer cells.
- Hormone therapy. Blocks cancer cells from getting the hormones they need to grow.
How Do Black Men Respond to Treatment?
Scientists don’t know if certain prostate cancer treatments work better for men of different races. But there’s evidence that Black men do just as well or better than men of other races when the same kind of care is available.
Black men with prostate cancer that hasn’t spread to other parts of the body (called nonmetastatic) tend to live just as long as white men when both groups get the same kind of treatment. Radiation therapy may work better for Black men with early prostate cancer. And hormone-based therapy may be more effective for Black men with metastatic castration-resistant prostate cancer (mCRPC). That’s a type of aggressive prostate cancer that no longer responds well to testosterone-lowering therapy.
Make sure your doctor goes over all your treatment choices. Black men with aggressive prostate cancer can benefit from surgery or radiation therapy. But they’re less likely than other races to get it. If your doctor doesn’t suggest these treatments, ask them why.
STATISTICS FOR PEOPLE OF COLOR
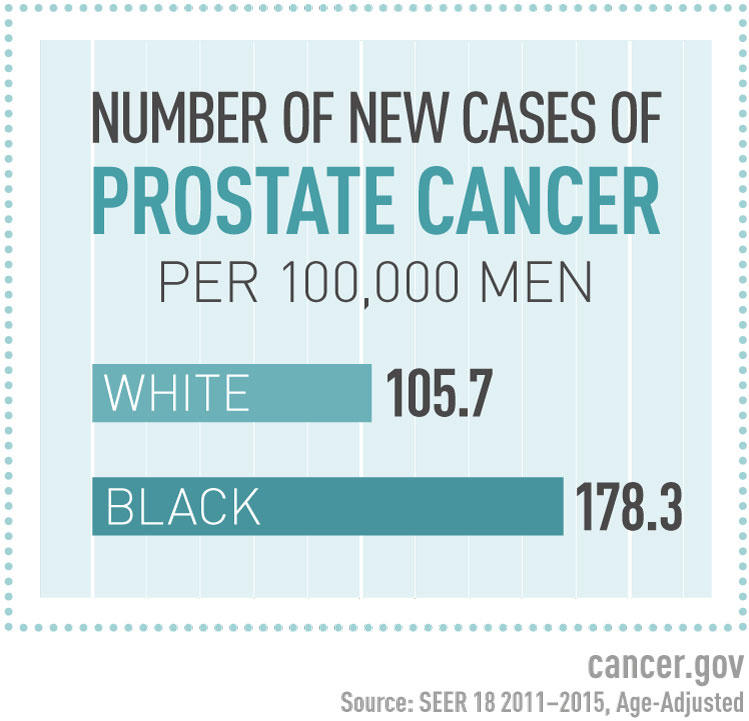
- All men are at risk for prostate cancer, but African American men are more likely to get prostate cancer than other men.
- Compared with white men, African American are twice as likely to die from the disease.
- African American men get prostate cancer at a younger age, tend to have more advanced disease when it is found, and tend to have a more severe type of prostate cancer than other men.
- Other than skin cancer, prostate cancer is the most common cancer in American men. The American Cancer Society’s estimates for prostate cancer in the United States for 2022 are:
- About 268,490 new cases of prostate cancer
- About 34,500 deaths from prostate cancer
Learn more about the Stats at GRAAHI's Health Equity Index
Links, Tools, Resources
Websites
https://www.mskcc.org/news/things-black-men-should-know-about-prostate
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2569237/
Latest Advances and Research in Prostate Cancer
https://www.cancer.gov/types/prostate/research
https://www.cityofhope.org/attacking-prostate-cancer-latest-weapons
Grand Rapids/Kent County/Michigan Resources
http://www.westmichpha.org/important-resources/the-survivors-association
https://vitalstats.michigan.gov/osr/Cancer/Race/Kent_Num.asp