Maternal & Infant health
Maternal deaths are preventable when symptoms are noticed and addressed early on.
Maternal & Infant Health
saving precious lives
Maternal deaths are preventable when symptoms are noticed and addressed early on.
What is MATERNAL & INFANT HEALTH?
- Maternal health refers to the health of a mother during and after pregnancy.
- Pregnancy can provide an opportunity to identify existing health risks in women and to prevent future health problems for women and their children.
- Black women are disproportionately affected by adverse events while pregnant.
- Many maternal deaths are preventable when symptoms are noticed and addressed early on.
symptoms
- New lump in the breast or underarm (armpit).
- Thickening or swelling of part of the breast.
Irritation or dimpling of breast skin. - Redness or flaky skin in the nipple area or the breast.
- Pulling in of the nipple or pain in the nipple area.
- Nipple discharge other than breast milk, including blood.
- Any change in the size or the shape of the breast.
- Pain in any area of the breast.
Risk Factors
- Getting older
- Genetic mutations
- Having dense breasts.
- Personal history of breast cancer
- Family history of breast or ovarian cancer
Ways to Prevent
There are many factors that can influence your risk of developing breast cancer of the course of a lifetime, however, there are things that can be done to help lower the risk, such as:
- Maintaining a healthy weight.
- Staying active.
- Limiting alcohol consumption.
- Breastfeeding your children, if possible.
If you have a genetic predisposition or are taking any medications that may increase your risk, talk to your physician to determine to best course of action to help lower your risk.

High Risk Pregnancy
Factors that can lead to a high risk pregnancy
- Advanced maternal age. Pregnancy risks are higher for mothers older than age 35.
- Smoking cigarettes, using marijuana, drinking alcohol, and using illegal drugs can harm the baby’s development.
- Maternal health problems. Existing conditions including hypertension, diabetes, obesity, and heart/blood disorders can increase the risk of pregnancy.
Pregnancy complications.
This can include conditions such as an ectopic pregnancy (the fetus grows outside the uterus), Rh sensitivity (your blood group is Rh negative and your infant’s blood group is Rh positive), and other possible complications.
Pregnancy history.
If you had preeclampsia in a previous pregnancy, you are more likely to develop it during the next pregnancy. If you have had a premature birth in a past pregnancy, you are more likely to have another one in your next pregnancy.
Steps to take to promote a healthy pregnancy
- Schedule a preconception appointment with your primary care provider. They will discuss with you things like how an existing medical condition can affect pregnancy and the risk of having a baby with a genetic condition.
- Go to regular prenatal visits so that your health and your baby’s health can be monitored. Your body will be undergoing many changes so frequent visits with your doctor are important.
- Take prenatal vitamins. Iron and folic acid (a B vitamin) supplements can prevent pregnancy related anemia. Folic acid supplements can also prevent major birth defects. It is advised to take a vitamin with 400 mcg of folic acid every day before and during pregnancy.

Breastfeeding your infant
Breastfeeding is essential because human milk provides the most complete form of nutrition for infants.
- Breast milk is easy to digest and has antibodies that can protect your baby from bacterial and viral infections.
- Breastfeeding benefits both your and your baby!
- Benefits for the infant include a reduced risk of asthma, obesity, type 1 diabetes, severe lower respiratory disease, ear infections, sudden infant death syndrome (SIDS).
- Benefits for the mother include a reduced risk of high blood pressure, type 2 diabetes, ovarian cancer, and breast cancer.
- There are a few situations when it is suggested not to breastfeed your infant. This includes if you have HIV. Since HIV can be spread through breast milk, mothers who have HIV should not breastfeed their infants.
Common Testing Tools
An ultrasound uses high-frequency sound waves to produce images of a baby in the uterus. It can be used to determine the gestational age of the baby and detect atypical development. It can also be used to measure the length of your cervix to determine if you’re at risk of preterm labor.
Prenatal cell-free DNA (cfDNA) screening is done to determine if the baby has an increased risk for specific chromosomal problems. It is done by using a maternal blood sample to screen fetal DNA.
Lab tests are done to test your urine for urinary tract infections and screen you for diseases such as HIV and syphilis.
Newborn screening is done within 48 hours of your baby’s birth. A sample of blood taken from a “heel stick” is tested for treatable diseases. This includes certain genetic, endocrine, and metabolic disorders, hearing loss, and critical congenital heart defects.
What to do once you're pregnant?
- Visit your primary care provider for a preconception appointment. If you are trying to become pregnant and when you become pregnant you will see an OB-GYN.
- An Obstetrician-Gynecologist (OB-GYN) is a doctor who specializes in women’s health.
- An Obstetrician (OB) cares for a woman during maternity. This includes pregnancy, labor, childbirth, and the postpartum period.
- A Gynecologist (GYN) cares for women at all stages of life, with a focus on the reproductive system.
- Most physicians specializing in women’s health are both an OB and GYN. They are referred to as an OB-GYN
- Look at your local Doula groups. The doula is a professional trained in childbirth who provides emotional, physical, and educational support to a mother who is expecting, is experiencing labor, or has recently given birth. Their purpose is to help women have a safe, memorable, and empowering birthing experience.

Common conditions that arise during pregnancy
High blood pressure (hypertension)
- A mother’s high blood pressure can make it hard for the baby to get enough oxygen and nutrients. Thus, if you know you have chronic hypertension, it is important to talk with your doctor and get it under control before you become pregnant.
Types of hypertension:
- Chronic hypertension: diagnosed before you get pregnant or before 20 weeks of pregnancy
- Gestational hypertension: diagnosed after 20 weeks of pregnancy or close to delivery. You only have high blood pressure during pregnancy and do not have protein in your urine or heart or kidney problems. Although it usually goes away after you give birth, having gestational hypertension can increase your risk of developing chronic hypertension.
- Preeclampsia: happens when a woman with normal blood pressure suddenly develops high blood pressure.
- Eclampsia: happens when a woman with preeclampsia develops seizures.
- Possible complications resulting from high blood pressure:
- For the mother: preeclampsia, eclampsia, stroke, the need for labor induction, and placental abruption (the placenta separates from the wall of the uterus).
- For the baby: preterm delivery and low birth weight.
Prevention:
- Keep a healthy weight through healthy eating and regular physical activity
- Use a home blood pressure monitor to keep track of your blood pressure at home and contact your doctor if your blood pressure is higher than usual
- Preeclampsia
- Preeclampsia happens when a woman with normal blood pressure suddenly develops high blood pressure and protein in her urine or other problems after 20 weeks of pregnancy. Women who have chronic hypertension can get preeclampsia.
- Symptoms: (Some women have no symptoms. That is why it is important to visit your healthcare provider regularly.)
- Persistent headache
- Changes in vision (blurry, seeing spots, etc)
- Pain in upper stomach area
- Nausea or vomiting
- Swelling of the face or hands
- Sudden weight gain
- Trouble breathing
Risk factors:
- This is your first birth
- You had preeclampsia during a previous pregnancy
- You have chronic hypertension, chronic kidney disease, or both
- You have a history of thrombophilia (a condition that increases risk of blood clots)
- You are pregnant with multiple babies (twins or triplets)
- You became pregnant using in vitro fertilization
- You have a family history of preeclampsia
- You have type 1 or type 2 diabetes
- You have obesity
- You have lupus (an autoimmune disease)
- You are older than 40
Gestational diabetes
- Gestational diabetes is a type of diabetes that occurs when your body can’t make enough insulin during your pregnancy. Insulin is needed to convert sugar and starches into energy. When your insulin levels are low, extra sugar can build up in the blood. This can increase the risk of birth defects in the baby and complications in the mother.
- Gestational diabetes is diabetes that is first seen in a woman who did not have diabetes before she was pregnant. Although gestational diabetes usually goes away after the baby is born, it does greatly increase your risk of developing type 2 diabetes later in life.
- Symptoms: Besides increased thirst and more-frequent urination, gestational diabetes doesn’t cause noticeable signs or symptoms. Thus, it is tested for between weeks 24 and 28 of pregnancy.
Risk factors:
- Being overweight or obese
- Not being physically active
- Having prediabetes
- Having had gestational diabetes during a previous pregnancy
- Having an immediate family member with diabetes
- Having previously delivered a baby weighing more than 9 pounds
Possible complications resulting from gestational diabetes:
- The baby can become extra-large (weigh more than 9 pounds) due to overfeeding. This can cause discomfort for the mother during the last few months of pregnancy and problems for both the mother and baby during delivery.
- Increased likelihood of a C-section delivery. When the baby is delivered via C-section, it takes longer for the mother to recover.
- Women with diabetes have high blood pressure (preeclampsia) more often than women without diabetes.
- If the diabetes is not well controlled during pregnancy, the baby can develop low blood sugar (hypoglycemia) after birth.
- Prevention and gestational diabetes management:
- Eat healthy foods including lean meat and proteins, dark green vegetables, whole grains, and healthy fats
- Exercise regularly (after checking with your doctor). Most women can exercise regularly during and after pregnancy. Get at least 30 minutes of moderate-intensity physical activity at least five days a week. This can include brisk walking, swimming, or playing with children.
- Monitor blood sugar often. Blood sugar levels change very quickly when you are pregnant.
- If insulin is ordered by your doctor, take it as directed.
- Get tested for diabetes 6 to 12 weeks after your baby is born, and then every 1 to 3 years. Half of all women who had gestational diabetes develop type 2 diabetes later in life.
Iron deficiency anemia
- Anemia is a condition that occurs when your body does not make enough healthy red blood cells or the blood cells do not work correctly. Someone who has iron deficiency anemia does not have enough iron in their body to make hemoglobin, which is the part of the red blood cell that carries oxygen through blood to the organs.
- Iron deficiency anemia affects more women and is most common in those who are pregnant. This is because more iron is needed during pregnancy to support the baby’s development. If iron deficiency anemia is not treated, it can raise your risk of a premature birth or low birth weight baby.
- Symptoms: (Iron deficiency anemia often develops slowly. At first, you may not have any symptoms or they may be mild.)
- Fatigue (very common)
- Weakness (very common)
- Dizziness
- Headaches
- Low body temperature
- Pale or yellow “sallow” skin
- Rapid or irregular heartbeat
- Shortness of breath or chest pain, especially with physical activity
- Brittle nails
- Pica (unusual cravings for ice, very cold drinks, or non-food items like dirt or paper)
- Prevention:
- Eat more food containing iron such as lean meat and chicken, dark, leafy vegetables (collard greens, spinach), and beans.
- Eat more foods that help your body absorb iron such as oranges, broccoli, strawberries, tomatoes, and other fruits and vegetables containing vitamin C.
- Avoid drinking coffee or tea with meals as these drinks make it harder for your body to absorb iron.
- Take a daily prenatal vitamin with 27 mg of iron or, if advised by your doctor, take an iron supplement.
Human immunodeficiency virus (HIV)
- HIV is a virus that attacks the body’s immune system. If the mother has HIV, it can be passed to the child anytime during pregnancy, childbirth, and breastfeeding.
- All women who are trying to become pregnant or are pregnant should get tested for HIV as soon as possible. If you have HIV, the sooner you start treatment the better.
- If you have HIV, the risk of transmitting HIV to your child can be less than 1% if you:
- Take HIV medication as prescribed through pregnancy, labor, and delivery
- Give HIV medicine to your baby for 4-6 weeks after birth
- How to prevent HIV transmission from mother to child:
- Take HIV medication as prescribed by your doctor. HIV medication reduces the amount of HIV in the body (viral load) to a very low, undetectable amount. This protects your baby, your partner, and yourself.
- If your HIV viral load is not low enough, a C-section delivery can help prevent HIV transmission.
- Do not breastfeed or pre-chew food for your baby. Although an undetectable viral load reduces the risk of HIV transmission to your baby through breastfeeding, it does not eliminate it.
Postpartum depression
Postpartum depression is depression that occurs 1-3 weeks after having a baby. Feelings of postpartum depression are more intense and last longer than those of “baby blues” (a term used to describe the worry, sadness, and tiredness many women experience after having a baby). Unlike postpartum depression, “Baby blues” symptoms typically resolve on their own within a few days.
Symptoms of depression:
- Lasting sad, anxious, or “empty” mood.
- Feelings of hopelessness or pessimism.
- Feelings of guilt, worthlessness, or helplessness.
- Feelings of irritability or restlessness.
- Loss of interest in hobbies and activities.
- Loss of energy.
- Problems concentrating, recalling details, and making decisions.
- Difficulty falling asleep or sleeping too much.
- Overeating or loss of appetite.
- Thoughts of suicide or suicide attempts.
- Aches or pains that do not get better with treatment.
- Symptoms of postpartum depression include those of depression and may also include:
- Crying more often than usual.
- Feelings of anger.
- Withdrawing from loved ones.
- Feeling numb or disconnected from your baby.
- Worrying that you will hurt the baby.
- Feeling guilty about not being a good mom or doubting your ability to care for the baby.
- Risk factors of postpartum depression
- Stressful life events.
- Low social support.
- Previous history of depression.
- Family history of depression.
- Difficulty getting pregnant.
- Being a mom to multiples (twins, triplets, etc).
- Being a teen mom.
- Preterm (before 37 weeks) labor and delivery.
- Pregnancy and birth complications.
- Treatment
- Talk to your healthcare provider and ask for a referral to a mental health professional.
- Your healthcare provider may suggest medication
- Join a support group of mothers also experiencing postpartum depression
STATISTICS FOR PEOPLE OF COLOR
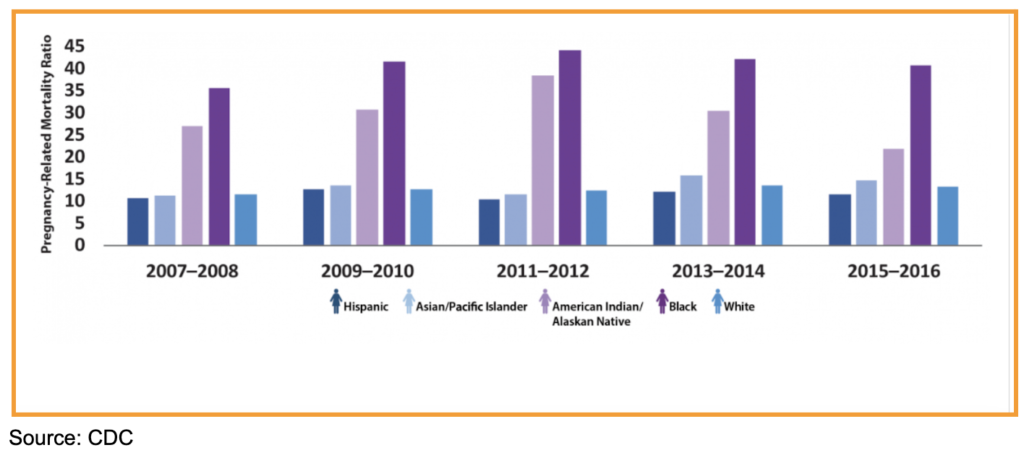
- The US maternal mortality rate increased from 20.1 deaths per 100,000 live births in 2019 to 23.8 deaths per 100,000 live births in 2020.
- In 2020, the maternal mortality rate for Black women was 55.3 deaths per 100,000 live births. This is 2.9 times the rate for non-Hispanic White women.
- The maternal death rate for Black or African-American (not Hispanic or Latina) women was 44.0 per 100,000 live births in 2019, then increased to 55.3 in 2020, and 68.9 in 2021.
- American Indian/Alaska Native and Black women are 2 to 3 times as likely to die from a pregnancy-related cause than white women.
Learn more about the Stats at GRAAHI's Health Equity Index
Links, Tools, Resources
Websites
https://www.cdc.gov/healthequity/features/maternal-mortality/index.html
https://www.nationalpartnership.org/our-work/health/reports/black-womens-maternal-health.html
https://blackmamasmatter.org/2023-black-maternal-health-week/
https://blackmaternalhealthcaucus-underwood.house.gov/Momnibus
https://www.cbpp.org/research/health/closing-the-coverage-gap-would-improve-black-maternal-health
https://www.healthaffairs.org/doi/10.1377/hlthaff.2022.00036
https://www.cdc.gov/reproductivehealth/maternal-mortality/index.html
Grand Rapids/Kent County/Michigan Resources:
https://www.spectrumhealth.org/healthier-communities/our-programs/maternal-infant-health-program
Sources:
https://www.cdc.gov/pregnancy/during.html
https://www.womenshealth.gov/a-z-topics/iron-deficiency-anemia
https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/high-risk-pregnancy/art-20047012