HIV/AIDS
The best way to reduce risk is to eliminate the stigma and know your status.
HIV/AIDS
Get Tested
The best way to reduce your risk is to eliminate the stigma, get tested and know prevention tools.
What is HIV/AIDS?
- HIV (human immunodeficiency virus) is a virus that attacks the body’s immune system. If HIV is not treated, it can lead to AIDS (acquired immunodeficiency syndrome).
- There is currently no effective cure. Once people get HIV, they have it for life.
- With proper medical care, HIV can be controlled. People with HIV who get effective HIV can live long, healthy lives and protect their partners.
Where did HIV originate from?
- HIV infection in humans came from a type of chimpanzee in Central Africa. Studies show that HIV may have jumped from chimpanzees to humans as far back as the late 1800s.
- The chimpanzee version of the virus is called simian immunodeficiency virus. It was probably passed to humans when humans hunted these chimpanzees for meat and came in contact with their infected blood.
- Over decades, HIV slowly spread across Africa and later into other parts of the world. The virus has existed in the United States since at least the mid to late 1970
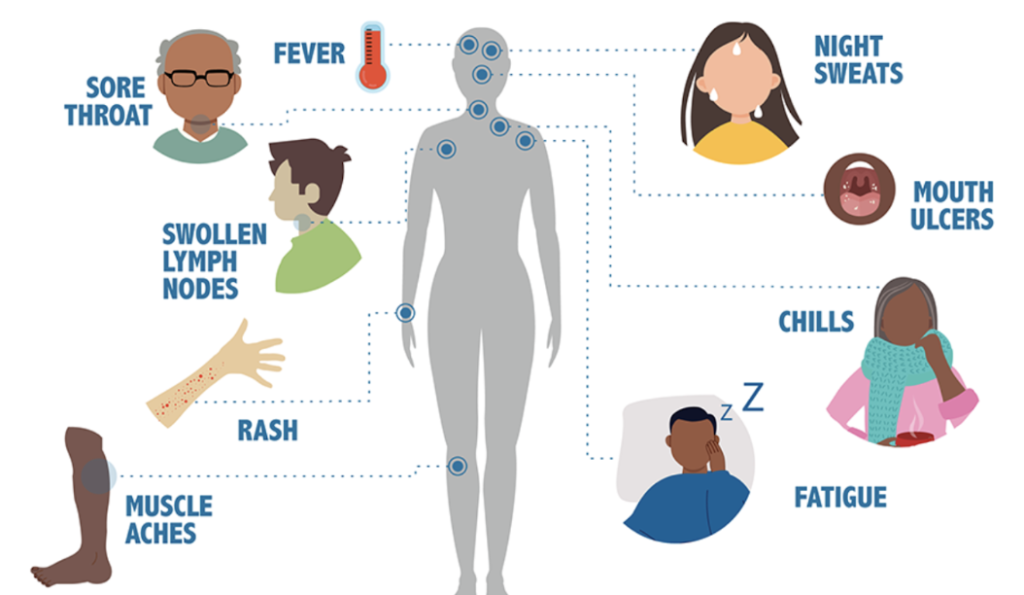
symptoms
Risk Factors
- Having condomless anal or vaginal sex
- Having another sexually transmitted infection (STI) such as syphilis, herpes, chlamydia, gonorrhoea and bacterial vaginosis
- Engaging in harmful use of alcohol and drugs in the context of sexual behaviour
- Sharing contaminated needles, syringes and other injecting equipment and drug solutions when injecting drugs
- Receiving unsafe injections, blood transfusions and tissue transplantation, and medical procedures that involve unsterile cutting or piercing
- Experiencing accidental needle stick injuries, including among health workers
Ways to Prevent
- Choose sex that is less risky than anal or vaginal sex. There is little to no risk of getting HIV through oral sex.
- You can’t get HIV from sexual activities that don’t involve contact with body fluids (semen, vaginal fluid, or blood).
- Condoms are highly effective in preventing HIV and other sexually transmitted diseases (STDs), like gonorrhea and chlamydia.
- Use water-based or silicone-based lubricants to help prevent condoms from breaking or slipping during sex.
- PrEP (pre-exposure prophylaxis) is a medicine people at risk for HIV take to prevent HIV.
- If taken as prescribed, PrEP is highly effective for preventing HIV from sex.
- PrEP is much less effective when it is not taken as prescribed.
- Not having sex (also known as being abstinent) is a 100% effective way to make sure you won’t get HIV through sex.
- If you have another STD, you are more likely to get HIV. Getting tested and treated for other STDs can lower your chances of getting HIV.
- If Your Partner Has HIV, Encourage Your Partner to Get and Stay in Treatment
Prevention Tools
PrEP and PEP are two ways to use anti-HIV medications as ‘prophylaxis’, in other words as prevention. They work in different ways. PrEP stands for pre-exposure prophylaxis. PEP stands for post-exposure prophylaxis. As indicated by ‘pre’, you start to take it before you may be exposed to HIV

Testing
The only way to know your HIV status is to get tested.
CDC recommends everyone between the ages of 13 and 64 get tested for HIV at least once.
Types of Testing
An antibody test looks for antibodies to HIV in your blood or oral fluid.
- Most rapid tests and the only HIV self-test approved by the U.S. Food and Drug Administration (FDA) are antibody tests.
- In general, antibody tests that use blood from a vein can detect HIV sooner than tests done with blood from a finger stick or with oral fluid.
An antigen/antibody test looks for both HIV antibodies and antigens.
- Antigen/antibody tests are recommended for testing done in labs and are common in the United States. This lab test involves drawing blood from a vein.
- There is also a rapid antigen/antibody test available that is done with blood from a finger stick.
A NAT(Nucleic Acid Test) looks for the actual virus in the blood.
- With a NAT, the health care provider will draw blood from your vein and send the sample to a lab for testing.
- This test can tell if a person has HIV or how much virus is present in the blood (HIV viral load test).
- A NAT can detect HIV sooner than other types of tests.
This test should be considered for people who have had a recent exposure or a possible exposure and have early symptoms of HIV and who have tested negative with an antibody or antigen/antibody test.
Timing of HIV Test Results
- HIV self-tests provide results within 20 minutes.
- With a rapid antibody test, usually done with blood from a finger stick or with oral fluid, results are ready in 30 minutes or less.
- The rapid antigen/antibody test, done with blood from a finger stick, takes 30 minutes or less.
- It may take several days to receive your test results with a NAT or antigen/antibody lab test.
What does an HIV diagnosis mean?
- If you receive an HIV diagnosis, it means that you have HIV.
- Unlike some other viruses, the human body can’t get rid of HIV completely. Once you have HIV, you have it for life.
- But with proper medical care, HIV can be controlled. People with HIV who get effective HIV treatment can live long, healthy lives and protect their partners.
What should I do if I just got diagnosed with HIV?
- Take Time to Process the News
- Receiving an HIV diagnosis can be life changing. You may feel many emotions—sadness, hopelessness, or anger.
- Allied health care providers and social service providers can help you work through the early stages of your diagnosis. They are often available at your health care provider’s office.
Stages of HIV & Transmission
Stage 1 – Acute HIV Infection
- People have a large amount of HIV in their blood and are very contagious.
- Many people have flu-like symptoms.
- If you have flu-like symptoms and think you may have been exposed to HIV, get tested.
Stage 2 – Chronic HIV Infection
- This stage is also called asymptomatic HIV infection or clinical latency.
- HIV is still active and continues to reproduce in the body.
- People may not have any symptoms or get sick during this phase but can transmit HIV.
- People who take HIV treatment as prescribed may never move into Stage 3 (AIDS).
- Without HIV treatment, this stage may last a decade or longer, or may progress faster. At the end of this stage, the amount of HIV in the blood (viral load) goes up and the person may move into Stage 3 (AIDS).
Stage 3 – Acquired Immunodeficiency Syndrome (AIDS)
- The most severe stage of HIV infection.
- People with AIDS can have a high viral load and may easily transmit HIV to others.
- People with AIDS have badly damaged immune systems. They can get an increasing number of opportunistic infections or other serious illnesses.
- Without HIV treatment, people with AIDS typically survive about three years.
Transmission of HIV
- Most people get HIV through anal or vaginal sex, or sharing needles, syringes, or other drug injection equipment.
- You can get HIV if you have anal sex with someone who has HIV without using protection (like condoms or medicine to treat or prevent HIV).
- Anal sex is the riskiest type of sex for getting or transmitting HIV.
- Being the receptive partner (bottom) is riskier than being the insertive partner (top).
- The bottom’s risk is higher because the rectum’s lining is thin and may allow HIV to enter the body during anal sex.
- The top is also at risk. HIV can enter the body through the opening at the tip of the penis (urethra); the foreskin if the penis isn’t circumcised; or small cuts, scratches, or open sores anywhere on the penis.
- You can get HIV if you have vaginal sex with someone who has HIV without using protection (like condoms or medicine to treat or prevent HIV).
- Vaginal sex is less risky for getting HIV than receptive anal sex.
- Either partner can get HIV during vaginal sex.
- HIV can enter a person’s body during vaginal sex through the delicate tissue that lines the vagina and cervix.
- Vaginal fluid and blood can carry HIV, which can pass through the opening at the tip of the penis (urethra); the foreskin if the penis isn’t circumcised; or small cuts, scratches, or open sores anywhere on the penis.
Other Possible Ways of Transmission of HIV
- Mother-to-child transmission is the most common way that children get HIV.
- Used needles, syringes, and other injection equipment may have someone else’s blood on them, and blood can carry HIV.
- People who inject drugs are also at risk for getting HIV.
- Engaging in risky sexual behaviors like having sex without protection (such as condoms or medicine to prevent or treat HIV).
- Oral sex involves putting the mouth on the penis (fellatio), vagina or vulva (cunnilingus), or anus (rimming). Factors that may affect the risk of getting HIV include ejaculation in the mouth with oral ulcers, bleeding gums, or genital sores
What are some rare ways that HIV has been transmitted?
- Workplace:
- The most likely cause is injury with a contaminated needle or another sharp object.
- Medical Care:
- The US blood supply and donated organs and tissues are thoroughly tested. It is very unlikely that you would get HIV from blood transfusions, blood products, or organ and tissue transplants.
- Food Contamination:
- The only known cases are among infants. Contamination occurs when blood from a caregiver’s mouth mixes with pre-chewed food and infant eats it.
What body fluids transmit HIV?
- blood,
- semen (cum),
- pre-seminal fluid (pre-cum),
- rectal fluids,
- vaginal fluids, and
- breast milk
These fluids must come in contact with a mucous membrane or damaged tissue or be directly injected into the bloodstream (from a needle or syringe) for transmission to occur. Mucous membranes are found inside the rectum, vagina, penis, and mouth.
Ways HIV is NOT transmitted
- HIV does not survive long outside the human body (such as on surfaces), and it cannot reproduce outside a human host. It is not transmitted.
- By mosquitoes, ticks, or other insects.
- Through saliva, tears, or sweat.
- By hugging, shaking hands, sharing toilets, sharing dishes, or closed mouth or “social” kissing with someone who has HIV.
- Through other sexual activities that don’t involve the exchange of body fluids (for example, touching).
- Through the air
LIVING WITH HIV
What do I need to do as part of my HIV care?
- Take Your HIV Medicine as Prescribed
- This will help keep your viral load low and your CD4 count high.
- Take your HIV medicine exactly how your health care provider tells you to—at specific times of the day, with or without certain kinds of food.
- Keep track of your medicine and schedule.
- Talk to your health care provider or pharmacist if you have questions about when or how to take your medicine, or if you are experiencing any side effects.
- Keep Your Medical Appointments
- Use a calendar to mark your appointment days.
- Set reminders on your phone.
- Download an app on your phone that can help remind you of your medical appointments.
- Keep your appointment card in a place where you will see it.
- Ask a family member or friend to help you remember your appointment.
- Talk Honestly with Your Health Care Provider
- Your health care provider needs to have the most accurate information to manage your care and treatment.
- Write down questions you want to discuss with your health care provider. Be ready to write down the answers.
- Keep track of your lab results, medical visits, and care and treatment plans.
- Make sure your health care providers have your correct contact information.
What can I expect during a medical visit?
- During your medical visit, your health care provider may ask questions and conduct routine medical exams to see how HIV is affecting your body.
- Your health care provider may
- Take a blood sample to check your viral load.
- Ask questions about your health history.
- Look for other kinds of infections or health problems. Some health problems may weaken your body, make your HIV worse, or prevent your treatment from working.
- Give you immunizations, if you need them.
- Discuss, prescribe, and monitor your HIV medicine.
- Discuss ways to help you follow your HIV treatment plan.
- Help identify other support you may need.
- Ask about your sexual or injection partners and discuss ways to protect them from getting HIV.
What are the different tests that help monitor my HIV?
- Your health care provider will use blood tests to monitor your HIV infection. These tests help your health care provider make decisions about changes to your treatment.
- CD4 Count
- Your CD4 count is the number of CD4 cells you have in your blood. CD4 cells help your body fight infections.
- HIV attacks and lowers the number of CD4 cells in your blood. This makes it difficult for your body to fight infections.
- Your health care provider will check your CD4 count every 3 to 6 months.
- Viral Load Test
- Viral load is the amount of HIV in your blood.
- Your health care provider will use a viral load test to determine your viral load.
- When your viral load is high, you have more HIV in your body. This means your immune system is not fighting HIV very well.
- You should have a viral load test
- every 4 to 6 months,
- before you take a new HIV medicine, and
- around 2 to 8 weeks after starting or changing medicine.
STATISTICS FOR PEOPLE OF COLOR
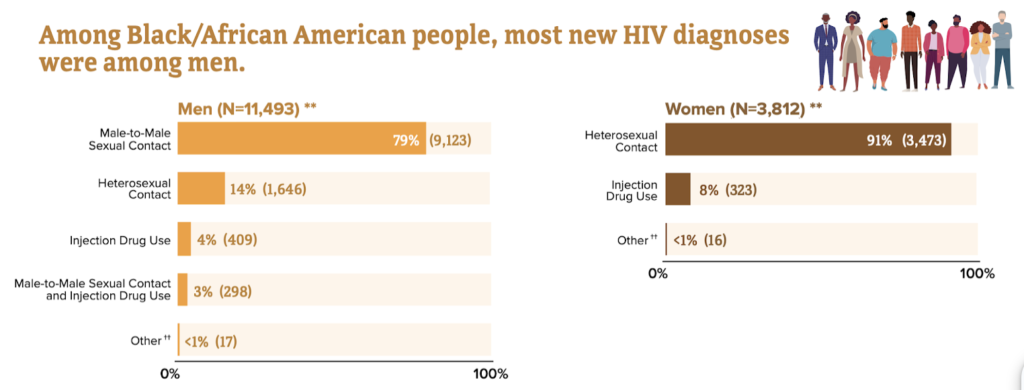
- Black/African American people account for a higher proportion of new HIV diagnoses and people with HIV, compared to other races and ethnicities.
- In 2019, an estimated 1.2 MILLION PEOPLE had HIV. Of those, 479,300 were Black/ African American people.
Learn more about the Stats at GRAAHI's Health Equity Index
Links, Tools, Resources
https://www.cdc.gov/hiv/basics/hiv-stigma/index.html
https://www.cdc.gov/hiv/basics/livingwithhiv/mental-health.html
https://www.cdc.gov/hiv/basics/livingwithhiv/healthy-living.html
https://www.cdc.gov/hiv/basics/livingwithhiv/resources.html
https://www.cdc.gov/hiv/basics/covid-19.html
Grand Rapids/Kent County/Michigan Resources:
https://redproject.org/services/hiv-case-management/
https://www.findhelp.org/health/hiv-treatment–grand-rapids-mi
https://www.michigan.gov/mdhhs/keep-mi-healthy/chronicdiseases/hivsti
https://aidsvu.org/local-data/united-states/midwest/michigan/
https://www.accesskent.com/Health/PersonalHealth/default.htm
Latest Advances, Clinical Trials & Breakthroughs in HIV/AIDS
https://insidescientific.com/milestones-and-recent-advances-in-hiv-research/
https://www.news-medical.net/health/Recent-Advancements-in-Treating-HIV.aspx